Clinical Data as An Asset to Transform HEDIS®
Quality Reporting & Care Gap Closure
Quality Reporting & Care Gap Closure
The goal of quality measurement is to consistently capture and report quality measure rates to provide benchmarks that drive healthcare towards patient-centered, high-quality care delivery. NCQA’s HEDIS® (Health Effectiveness Data and Information Set) is healthcare’s largest quality reporting program. To maximize compliance and quality improvement, incorporating clinical data into HEDIS reporting should be a high priority for health plans.
Many quality measures leverage claims data, chart abstractions, and registries to report and measure compliance across process and outcome measures. But more healthcare information is being generated year-over-year and supplemental data for quality reporting from electronic health records (EHR) is now top of mind for regulatory organizations, such as the Centers for Medicare & Medicaid Services (CMS), as well as payers and provider organizations. Clinical data, captured at the point of care, can be used to organically demonstrate care quality, and should automatically be incorporated in quality measures to show compliance and improve the timeliness and accuracy of reporting.
However, HEDIS measure reporting today still requires extra work from clinicians and administrators to ensure that data complies with strict coding standards and can be processed effectively by reporting engines. There is an opportunity for regulatory organizations, payers, providers, and solutions partners to shift measurement from an operational burden to an instrumental tool to equitably compare care quality across sites of care and enable more informed healthcare decisions.
“Upcycled Data from Availity can be used to close data gaps; reduce the administrative burden of HEDIS reporting; improve HEDIS compliance rates and boost Stars Ratings; and help proactively identify care gaps.”
This increases the accuracy of numerator values for measures that require vital signs or test results (such as glucose and blood pressure control), increasing compliance rates in tandem with care being delivered. Availity Fusion™, our API-based Upcycling Data™ technology, supports data upcycling by aggregating data from EHRs, health information exchanges (HIEs), labs, and other sources and then normalizing and enhancing it to deliver a consistent, standards-based data asset that’s ready for use. Upcycled Data from Availity can be used to close data gaps; reduce the administrative burden of HEDIS reporting; improve HEDIS compliance rates and boost Stars Ratings; and help proactively identify care gaps.

Background: HEDIS Quality Measures & The Digital Future HEDIS is used by more than 90% of health plans. Nearly 200 million people are enrolled in plans that report HEDIS results.¹ Billions of dollars are allocated based on HEDIS measures. Specifically,
For years, health plans relied solely on claims data to calculate HEDIS measures. The next generation of quality reporting involved hybrid measures, which used chart abstraction to glean clinical outcomes and supplement administrative data. Now, digital supplemental data from EHRs and other sources such as HIEs can be combined with claims to calculate performance on measures that require clinical information, such as test results or vital signs.
“Both CMS and NCQA have initiatives that are propelling the industry towards a digital quality future in which clinical data captured in EHRs can be reported once and used for multiple purposes. This will eliminate continuous requests for charts from payers to providers as well as dependence on manual chart abstraction, removing burden, cost, and time from quality management processes.”
As an example, the HEDIS measure for Controlling High Blood Pressure (CBP) focuses on adults aged 18-85 with a diagnosis of hypertension, where their blood pressure is adequately controlled (<140/90 mmHg). Standard diagnosis codes determine the denominator hypertensive population, while compliance in the numerator population is determined using standard vital sign codes and results. Vital signs can be recorded using CPTII codes like 3074F, which indicate systolic blood pressure <130 mmHg, or specific readings gathered from clinical sources.
Incorporating accurate, standards-adherent clinical information in quality measurement ensures the correct representation of closed gaps. If a healthcare provider uses a local, site-specific code to document evidence of hypertension in the medical record, the diagnosis may not be captured automatically in quality reporting. As a result, the patient may be excluded from the denominator of the above measure. This means the member is not only excluded from the HEDIS measure, representing it inaccurately, but they may be excluded from necessary disease management programs and excluded from care gap outreach workflow.
Over time, this one data gap can lead to poor health outcomes, low engagement, as well as avoidable cost and utilization. Another example is when a member with a hypertension ICD10 code diagnosis is included in the denominator, but their recent blood pressure readings are recorded in the EHR without units. This means the vital sign results cannot be used in the quality measure calculation and compliance is under-reported. Further, because the member is included in the denominator, but appears to have an open care gap, they may be incorrectly included in outreach, causing unnecessary workflow burden, duplicate services, and waste. This results in poor member experience and their engagement and satisfaction may decline over time.
Both CMS and NCQA have initiatives that are propelling the industry towards a digital quality future in which clinical data captured in EHRs can be reported once and used for multiple purposes. This will eliminate continuous requests for charts from payers to providers as well as dependence on manual chart abstraction, removing burden, cost, and time from quality management processes. Quality reporting will also be aligned with interoperability and data exchange standards, such as Fast Healthcare Interoperability Resources (FHIR.), which are being implemented across the industry for further efficiency.
Example initiatives include:
Clinical data is increasingly important for accurate, effective quality measurement to improve care – especially for patient-specific measures focused on outcomes. Clinical data can be timely, updated with recent and historical member information, and contains rich clinical elements, such as lab test results, vital signs, and physician notes, which are not present in other data sets. However, clinical data in its raw form poses considerable challenges. Availity and its affiliated companies have been in the business of standardizing and enriching clinical data for nearly a decade and has processed clinical data for more than 160 million individuals.
Our clinical informatics organization conducts data quality analyses as part of each deployment, including annual real-world data audits, and routinely finds that upwards of 50% of source clinical data cannot be used in its raw native form. A variety of factors contribute to this lack of immediate usability:
The following examples demonstrate how Availity Fusion’s upcycled clinical data, which is normalized and consistent with the HEDIS value set, can improve HEDIS reporting accuracy and enable identification of care gaps.

Value of Upcycled Data for Comprehensive Diabetes Control (CDC) – HbA1c

Value of Upcycled Data for Comprehensive Diabetes Control (CDC) – Blood Pressure
To get the most benefit from clinical data for HEDIS and quality improvement, organizations are investing in robust clinical data transformation and integration solutions. Availity Fusion’s comprehensive process to normalize, enrich, reorganize, deduplicate, and summarize multi-source, multi-format data in real time increases the usability of clinical data for HEDIS reporting as well as other digitally enabled use cases.

A sample study performed using multi-source clinical data processed through Availity Fusion demonstrated the following impact across clinical domains:
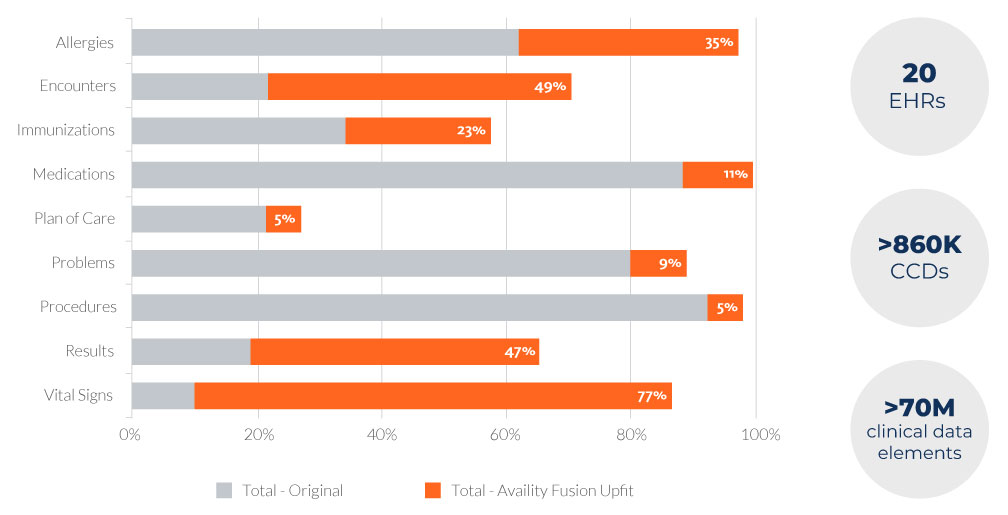
This impact was achieved through advanced transformations, such as normalizing free-text values to codified standards, converting values to standard units of measure, and reorganizing data to expected domains. The study determined that increased data normalization and standardization across domains translated to a higher yield of HEDIS numerator-specific data.
To better quantify the potential impact of Upcycled Data, Availity performed analysis with clients focusing on the clinical data elements relevant for HEDIS, and the following was observed:
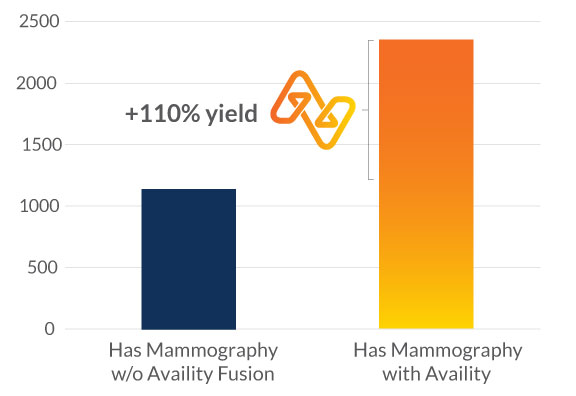
In an analysis of 27 months of source data related to breast cancer screening, 1,164 patients were found to have had a mammogram according to the value sets defined by the Breast Cancer Screening measure. After processing by Availity Fusion, 2,390 patients were identified to have had a mammogram, which represents a 110% yield over what was available in the original data prior to normalization.

Colorectal Cancer
Screening
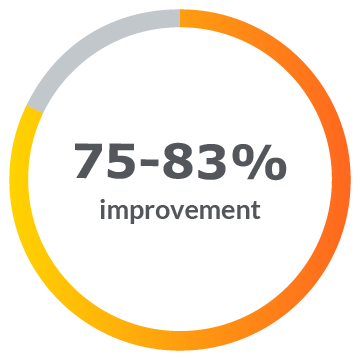
in standardized data elements usable for numerator compliance.

Breast Cancer
Screening
in standardized data
elements usable for numerator compliance.
Comprehensive
Diabetes Care (HbA1c)
in standardized data elements usable for numerator compliance.
Ultimately, the ability to capture and standardize critical elements of quality measures can help improve measure accuracy and may lead to enhanced CMS compliance rates. More broadly, plans leveraging this clinical data asset in quality measurement have the potential to effectively close care gaps and improve outcomes, reduce the burden of poor data quality on clinical staff, and improve the care experience of each member.

Availity Fusion supports data upcycling by aggregating data from EHRs, HIEs, labs, and other sources and then normalizing and enhancing it to deliver a consistent, standards-based data asset that’s ready for use. For HEDIS reporting and care gap identification, the data extraction pipeline pulls data from the Availity Fusion engine, filters for relevant data elements, and produces flat files for ingestion by HEDIS reporting engines. Availity’s HEDIS Extracts are a fit for purpose output, designed to increase accuracy and efficiency across HEDIS measurement by reporting engines. HEDIS engines can then calculate, measure, and submit quality compliance rates by processing data from clinical and claims sources. The data must be delivered in specific layouts using standard value sets, where these value sets are defined as groups of one or more standard clinical codes, such as LOINC, ICD-10-CM, SNOMED-CT, CPT, etc.
A national health plan customer performed a robust study to evaluate the impact of high-quality clinical data in HEDIS reporting accuracy. The plan reported up to 20% increases in measure compliance across HEDIS quality measures as a result of Upcycling Data through Availity Fusion. The output included standardized lab, procedure, and immunization elements that directly correlate to preventative screening measure specifications.
With an accurate picture of completed screenings, this health plan produced more accurate outreach reports for care gap closure, reduced duplication and waste, and improved member experience. Further, this insight empowered providers to manage the right members at the right time. Extracts can then be used as the source of clinical data for HEDIS engines to ingest and calculate HEDIS measure outcomes. If evidence towards a measure is coded in any format other than those identified in the value set, the evidence will not be counted towards the measure.
“With an accurate picture of completed screenings, this health plan produced more accurate outreach reports for care gap closure, reduced duplication and waste, and improved member experience.”
Availity Fusion’s normalization is critical to generating the highest volume of usable data for HEDIS reporting. Availity’s HEDIS Extracts are produced on a scheduled basis with incremental data included in each data extraction and a final output is provided for measure year reporting. Health plans have the ability to specify HEDIS measures of interest on a yearly basis and supply a member list for each data extraction, as needed. The data is filtered based on the numerator criteria and any required exclusions for the measures and delivered in the layout required by the HEDIS engine.
Member satisfaction has become more dominant, becoming 57% of Star Ratings as of 2023. A plan that understands the unique needs of each member and proactively manages members will help gain and maintain the trust of their membership and increase overall engagement, enrollment, and retention.
Today, health plans are going beyond simply paying for services. They are actively involved in orchestrating the best care at the lowest price for members. Upcycled clinical data contributes to more accurate care gap identification and clinical quality measurement in support of this expanded role. But the shift towards strategic use of clinical data for HEDIS requires an investment in clinical data acquisition and – equally important – an investment in technology to transform raw clinical data into an asset that is standard, organized, and actionable. The inherent variation in source documentation and accuracy, a plethora of custom and standard terminologies, and fragmented storage of data across the healthcare system all contribute to clinical data’s complexity.
Availity Fusion technology normalizes data to industry standard terminologies, consistent with the HEDIS value set, and outputs fit for purpose HEDIS Extracts to increase the accuracy of quality measurement. With a higher volume of usable data available for reporting and care gap identification, compliance and health outcomes improve in tandem.