About Atrium Health
Atrium Health is a leading nonprofit health system based in Charlotte, North Carolina, and part of Advocate Health, the third largest nonprofit system in the U.S. with 40 hospitals and over 1,400 care locations across the Southeast. Atrium Health is nationally recognized for its innovation in research, education, and patient care. Its academic partner, Wake Forest University School of Medicine, is a leader in medical education and research.
Challenge
Atrium Health, a long-time Availity client, uses Availity Revenue Cycle Management (RCM)—integrated within its Epic workflows to manage specialty claims, including Workers’ Compensation. While Availity’s electronic attachments module helped flag claims requiring documentation, the
review process remained heavily manual. Claims and attachments were frequently dropped to paper and routed to the Edit/Error Management queue, where staff manually reviewed and processed each submission. This paper-heavy workflow slowed operations, increased administrative workload, and created bottlenecks for the specialty billing team. Instead of focusing on high-priority claims, staff were spending time printing, bundling, and mailing documents contributing to a backlog of over $2 million in unresolved Workers’ Comp claims. The inefficiencies were also affecting days in A/R, straining cash flow, and pulling staff away from more strategic, value-generating tasks.
Solution
To address the growing backlog and operational inefficiencies, Atrium Health implemented automated batch attachments within Availity RCM. Previously, staff had to manually print, match, and mail documentation for claims that required attachments—a time-consuming process that contributed to significant delays and rising operational costs. With the new solution, teams could upload claims and related attachments in a single batch file. Availity RCM then automatically matched each attachment to its corresponding claim—delivering them electronically to payers that support EDI or dropping them to paper when required. The automation eliminated the need for manual intervention in the attachment process and integrated seamlessly with Atrium Health’s existing Epic-based workflows. This shift not only reduced administrative overhead and mailing costs but also freed up staff to focus on higher-value work, supported faster claims turnaround, and positioned the organization to scale more efficiently as volumes continued to grow.
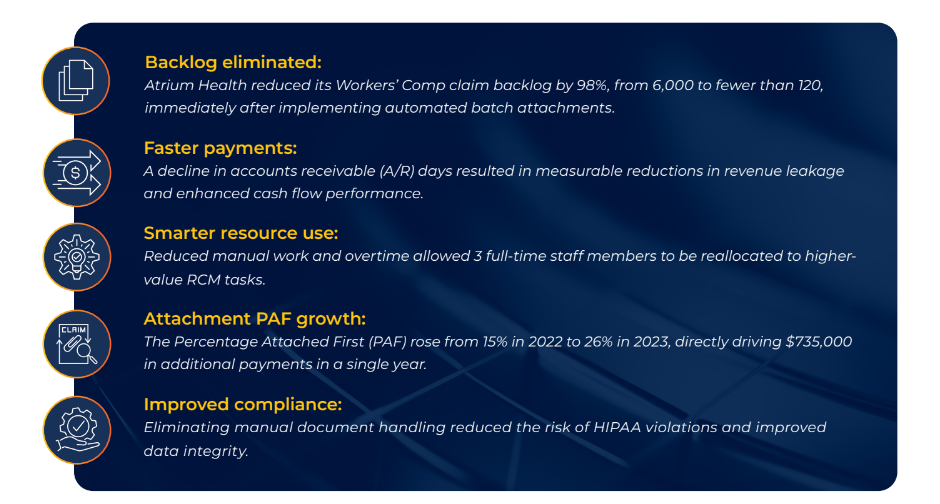
Results
By implementing automated batch attachments within Availity RCM, Atrium Health eliminated the need for manual routing through the Edit/Error queue, as well as time-consuming onsite printing and mailing. With minimal IT effort and no additional software investment, the organization transitioned to a digital-first workflow that improved speed, compliance, and staff efficiency.